The Department of Mental Health (DMH) transitioned into a new mental health payment model as of January 1, 2019. Mental Health Payment Reform has represented a large operational and cultural shift towards focusing on how well the public mental health system is doing rather than simply how much it is doing. The shift has given agencies more flexibility with funding to meet the needs of the children, youth, adults, and families they serve. By simplifying the baseline payment structures and adding Value-Based Payments that reward outcomes and incentivize best practices, DMH continues to aim to make it easier for mental health providers to meet the goal of efficient and effective care for Vermonters with mental health needs.
Mental Health Payment Reform is the culmination of a multi-step and iterative process co-produced by staff with relevant expertise, provider agencies, and other community partner organizations from across the system of care. Payment reform typically follows a four-step process which begins with planning and design and then moves through to initial implementation and ongoing evaluation. This initiative utilizes a multi-layer project governance structure, consisting of several subject matter specific work groups and a steering committee for work group report-outs and oversight of broad strategic project goals.
In total, the Department of Mental Health in collaboration with the Department of Vermont Health Access Payment Reform Unit engaged in over 150 hours of work group meetings over a 16-month period. More information and materials related to each mental health payment reform work group can be found below. In addition to the workgroup meetings, DMH and DVHA engaged with a variety of stakeholders, which included: AHS staff; Vermont Care Partners; Designated Agency Directors from CYFS, CRT, Financial, and Emergency Services; Designated Agency program managers and staff; Local Program Standing Committees; Local Interagency Teams; IFS Core Teams; Accountable Communities for Health; Consumer Advocacy Groups such as Medicaid Exchange Advisory Board; Department for Disabilities, Aging, and Independent Living Advisory Board; Developmental Services State Program Standing Committee; State Program Standing Committees for Children’s Mental Health and Adult Mental Health; Act 264 Advisory Board; Vermont Federation of Families for Children’s Mental Health; Mental Health Block Grant Planning Council; NAMI; and the Vermont Family Network.
Payment Model/Methodology & Business Operations:
The goal of the Payment Model and Methodology Work Groups is to create a value-based payment model for appropriate mental health services at Designated and Specialized Service Agencies that is able to adapt to changing programs, services, related payments, and caseload in ongoing years. This work group also focused on State and Designated Agency needs to operationalize the payment reform including updated business and program operations.
New Payment Model and Billing Changes
Accountability & Encounter Data:
The goal of the Accountability & Encounter Data workgroup is to identify mental health payment reform data requirements and operationalize changes to monitoring and reporting structures to ensure the integrity of mental health programs and services and meet Federal and State auditing requirements. In support of this goal, the work group performs the following tasks:
- Define minimum standards for mental health encounter data
- Define MSR & MMIS encounter data reporting requirements
- Update State and Federal reporting processes as needed
- Review program integrity standards, update as needed
Key Changes in the New Provider Manual
Quality & Program Evaluation:
The goal of the Quality and Program Evaluation group is to develop quality improvement measures and oversight and to develop frameworks to evaluate and evolve the payment model over time to ensure effectiveness and ongoing sustainability
- Develop a framework for State/DA payment model review (i.e., adding services, adding performance measures, and adjusting case rate as needed
- Develop a framework for federal payment model review
Steering Committee:
The goal of the Steering Committee is to offer a checkpoint for stakeholders across the various subject matter specific work groups to receive updates and ask questions about decisions made across the mental health payment reform project.
Overview
This page provides resources for Designated Agencies (DAs) and Specialized Services Agencies (SSAs) that enter into Provider Agreements with the Department of Mental Health (DMH).
Medicaid.gov
Vermont Global Commitment to Health 1115 Waiver
- Documents and Resources
- Global Commitment Register (Policy changes to and clarifications of existing Medicaid policy under Vermont's 1115 Waiver
Value-Based Payment (VBP) Performance Measures
Resources
For DAs:
For SSAs:
- CY2025 (NFI)
- CY2025 (Pathways Vermont)
- CY2024 (NFI)
- CY2024 (Pathways Vermont)
- CY2023 (NFI)
- CY2023 (Pathways Vermont)
Calendar Year 2025 Value-Based Payment Points Table
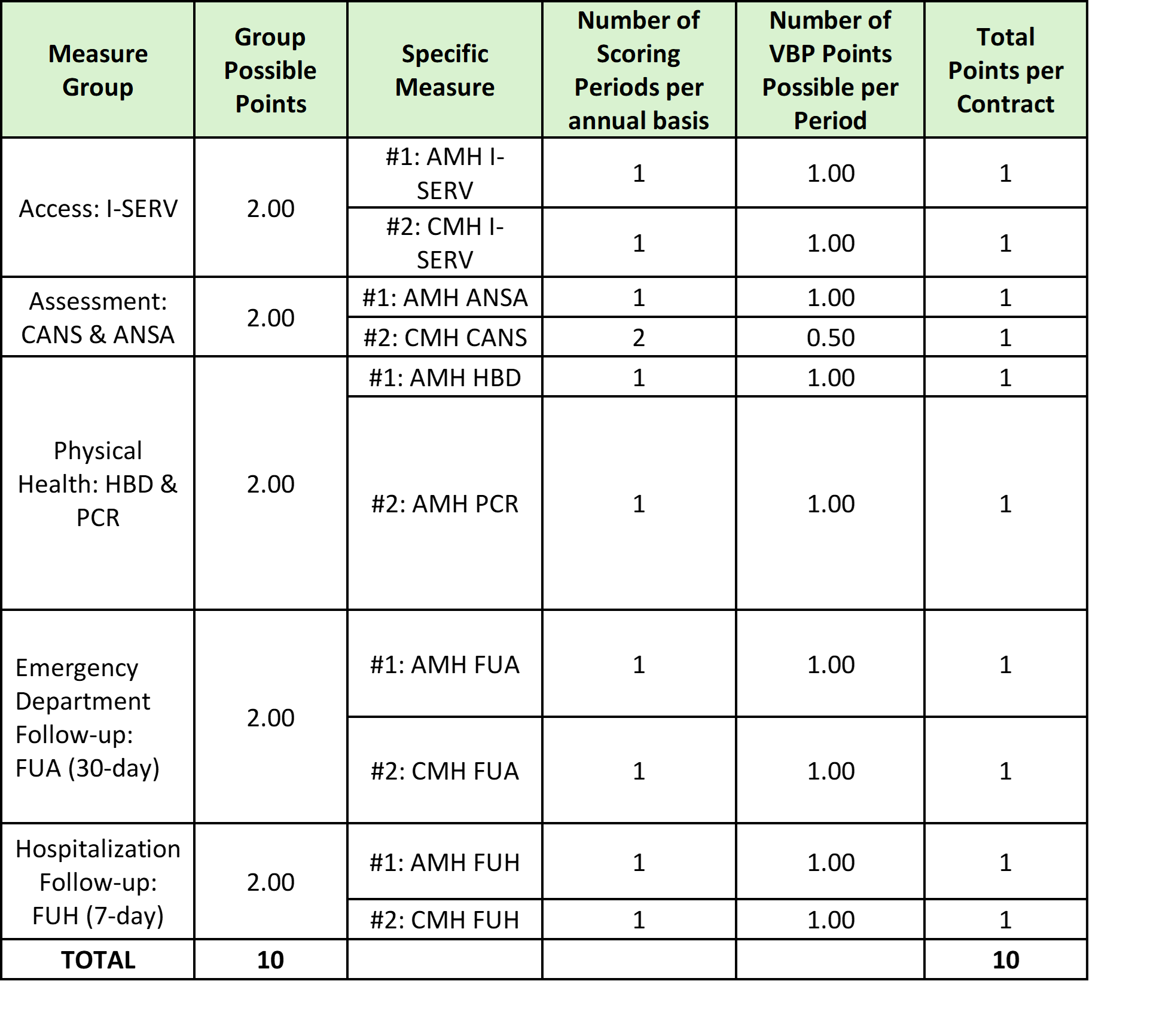
Calendar Year 2024 Value-Based Payment Points Table